Healthcare Revenue Cycle Management

Achieve your financial performance goals with optimized systems and expert teams. We have in-depth experience at every stage of the revenue cycle; our flexible, scalable strategic solutions are bespoke to the needs of healthcare business owners.
We’re incredibly proud of our growing customer base that comprises every healthcare specialty, including:
- Solo and group physician practices
- Surgical centers
- Laboratories
- Healthcare groups
- Urgent and in-patient treatment centers
- Large-scale health systems
AIMA – Experts in Healthcare Revenue Cycle Management
Healthcare revenue cycle management is the external financial services used by healthcare businesses to manage their administrative and clinical functions associated with claims processing, payment, and revenue generation. The process encompasses the identification, management, and collection of patient service revenue.
Operating for 25 years, we know that working within the healthcare sector brings variable challenges. Whether your focus is maximizing reimbursements, managing growth, maintaining strict standards against industry benchmarks, or building patient service initiatives. Whatever your challenges, AIMA is here to help.
Here at AIMA, we have an individual customer approach. Your dedicated account manager will build a long-standing collaborative relationship with you to gain a unique understanding of your business, its challenges and most importantly, its opportunities. We invest time and effort to help you succeed beyond only increasing revenue and cash flow. We work with you to develop plans for consolidating clinical and administrative systems, to integrate back-office operations which ultimately improve volumes, revenues and margins.
Compliance for all
Coding compliance and accurate billing are central to the long-term success of any healthcare business. Don’t leave proper documentation and reimbursement to guesswork when you see patients, perform exams, and test samples. All too often, paperwork and billing become an overwhelming complex regulatory process — and a single misstep can mean lost revenue, fines, or worse. At AIMA, we adopt a holistic approach to compliance, evident throughout all we do. Not just a bolt-on, an after-thought, or an up-sell service. Compliance for all, always.
Need Help?
Contact AIMA Business and Medical Support today. Our friendly team are on hand to answer your questions.
US (321)236-8300
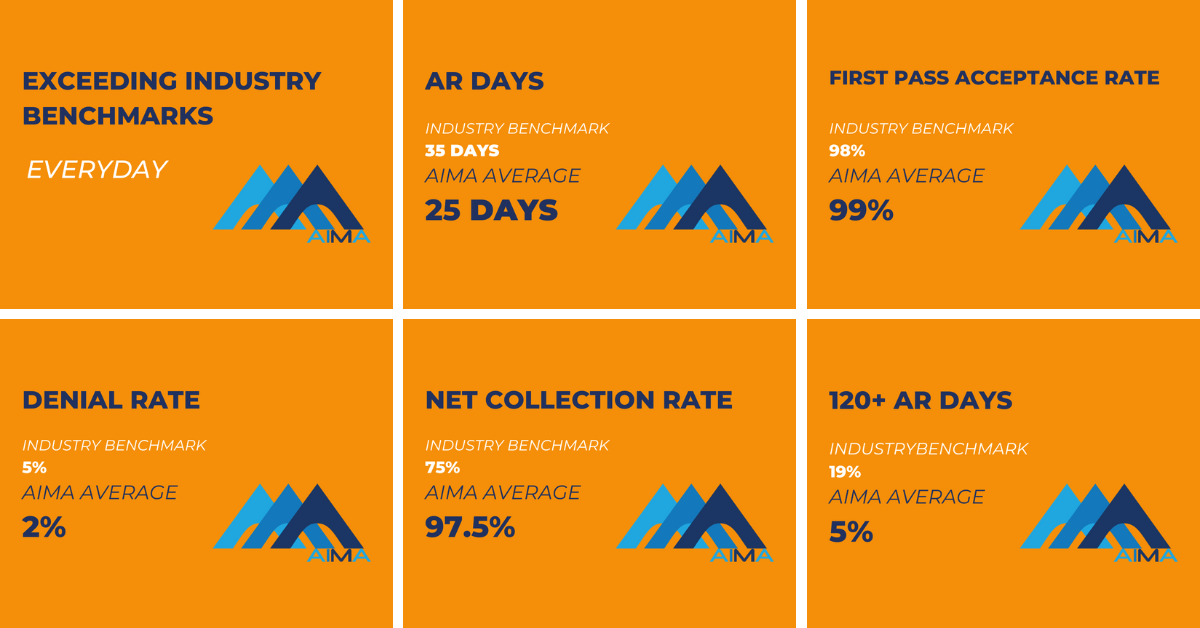
Our Healthcare Services Results

AIMA Healthcare Revenue Cycle Management Service
AIMA also has extensive experience and proven results in the following areas:

AIMA Technology Services

